TERMINOLOGY
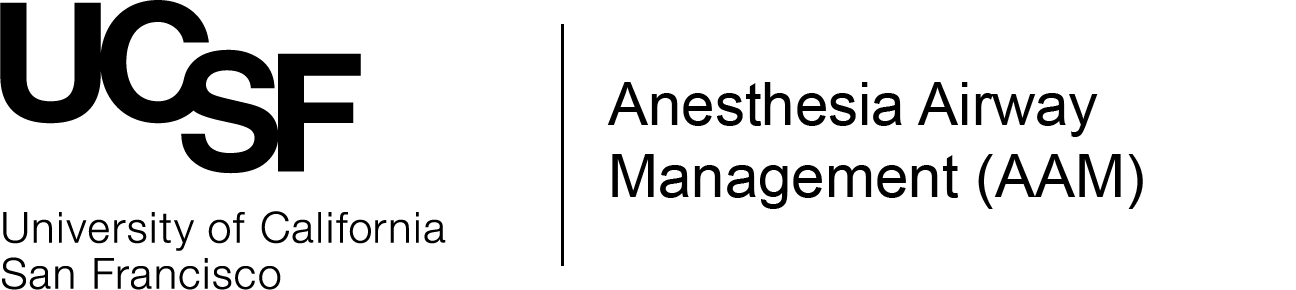
A number of terms such as FONA, front-of-neck airway, front-of-neck access, eFONA (emergency FONA), 'cric' (as in 'kraɪk'), or cricothyrotomy describe what is essentially the same thing: Access to the airway from the front of the neck. Generally, FONA is understood to mean access through the criothyroid membrane (CTM).
A tracheostomy is technically also a front-of-neck airway, but not through the cricothyroid membrane. Tracheostomy is discussed elsewhere.
INDICATIONS
There are two situations in which a FONA is indicated (the first one is the more relevant for the vast majority of anesthesia providers):
1. CICO (can't-intubate-can't-oxygenate) scenario
The classic indication for FONA is as a rescue technique for a CICO (can't-intubate-can't-oxygenate) scenario, which describes a situation when attempts at intubation and oxygenation with a facemask, airway adjuncts and/ or an SGA have been unsuccessful. If you find yourself in a CICO scenario the only available airway management option is a FONA! Therefore a FONA is the ultimate step in management algorithms for an unanticipated difficult airway when everything else has failed.
CAUTION: There is no such thing as an anticipated CICO scenario. If your preoperative airway assessment and planning suggests that CICO is likely after induction of general anesthesia, the airway needs to be secured awake!
It is quite possible that you will never have to perform a FONA for a CICO scenario during your professional career but since it is the only managment option for this scenario it is essential that you know relevant FONA techniques and their place in the management algorithm of the unexpected difficult airway.
2. 'Elective' FONA
In certain (rare) clinical scenarios an 'elective' FONA before induction of general anesthesia, i.e. in an awake patient, can be indicated. This could be a situation where surgery is required for a high-grade upper airway obstruction and conventional oral/ nasal and awake fiberoptic intubation are unlikely to be successful (as is BMV or an SGA). The 'go-to' technique in this setting is generally a tracheostomy under local anesthesia performed by an ENT surgeon, but cricothyrotomy (with a 'small-bore' device) has also been used by anesthesia providers in this situation. You are unlikely to encounter these approaches outside of very specialized practice settings with surgeon-anesthesiologist teams who are highly experienced in advanced airway management.
ANATOMY
A basic knowledge of the anatomy of the larynx and upper trachea and the relevant palpable landmarks are essential for identifying the cricothyroid membrane (CTM). Identifying the CTM is arguably the most important step of any cricothyrotomy technique.
Generally the only laryngeal landmark that is visible in some patients is the laryngeal prominence of the thyroid cartilage/ the thyroid notch ('Adam's apple'). Visually localizing the CTM is therefore unreliable. Consequently, Identifying the CTM relies on palpation. How to localize the CTM with palpation is described below under 'TECHNIQUE'. Ultrasound has been investigated as a means to find the CTM and is advantageous especially in obese patients. However, due to the time pressures in a CICO scenario it cannot be recommended as a standard of care in the emergent setting.
TIP: Practice finding the cricothyroid membrane! Make it a habit to every now and then palpate a patient's neck (after induction of general anesthesia) to identify the location of the CTM. You will come to appraciate that is is very easy to identify the cricothyroid membrane in some, and extremely diffcult in others. There is a huge degree of variability!
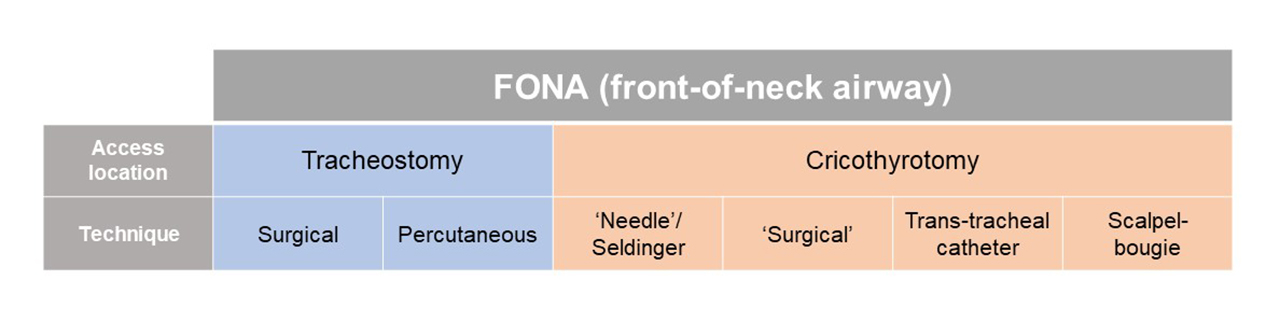
EQUIPMENT
Different equipment options exist for different technical approaches as described below. They range from pre-packaged kits containing purpose-designed tracheal cannulas to 'home-made' bougie/ scalpel/ ET tube packs.
TECHNIQUE
As a CICO rescue technique FONA has to be performed FAST! When you are starting the procedure the patient will most likely already be deeply hypoxic en-route to a hypoxic brain injury and cardiac arrest. The goal should be to perform a FONA in under 30 seconds.
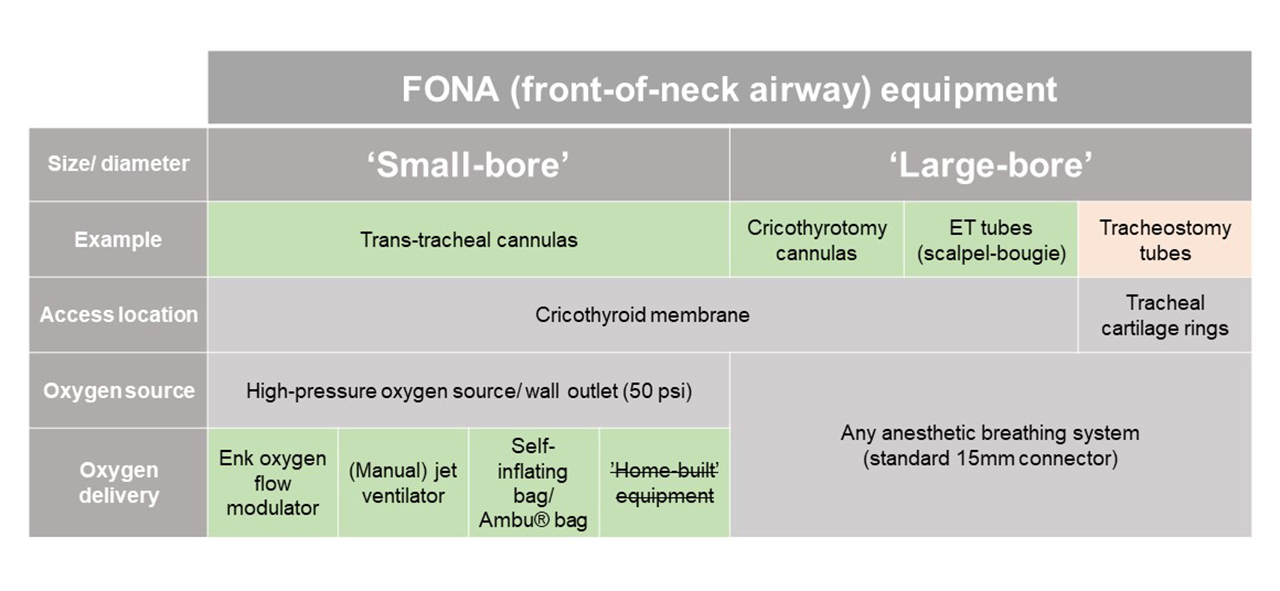
Airway management algorithms
Together with learning and practicing a FONA technique it is essential that you know when to use it, meaning you need to be familiar with an algorithm for managing the unexpected difficult airway. A number of algorithms have been published by various (national) specialist societies, including but not limited to guidance from the UK Difficult Airway Society or the American Society of Anesthesiologists (currently being reviewed for an update). A management algorithm which is widely taught and used in Australia is the Vortex approach. A recent overview of published management algorithms is given by Edelman et al. (2019).
NOTE: When reviewing the different technical approaches described below please note that many (slight) variations of these techniques have been described and used successfully.
Different techniques can be used to access the trachea through the cricothyroid membrane. Please click the links to view descriptions of available techniques:
'Needle'/ Seldinger FONA
'Surgical' FONA
Scalpel-bougie FONA
Trans-tracheal catheter FONA
CHALLENGES & CONTROVERSIES
Which technique ist 'best'?
One question that usually comes up when discussing various FONA techniques is 'Which one is best?'. This really depends on how you define 'best'? The best technique could be the one that is the fastest, the easiest to learn, the one that uses the most familiar or cheapest equipment, the one that needs the least amount of equipment, the one that has the highest success rate, or the one with the fewest complications. Ideally, the best technique would tick all of those boxes, but, of course no single technique does.
While there has arguably been a shift from recommending trans-tracheal cannula techiques (especially in conjunction with jet ventilation) towards 'surgical' approaches and the scalpel-bougie technique, there is ongoing debate over which is 'best' (Baker et al., 2016; Greenland et al., 2017).
How to practice and train for FONA?
While you obviously cannot justify practicing a complete FONA technique in a real patient, you can train certain parts of the technique, such as...
- Identifying the location of cricothyroid membrane through palpation (in anesthetized patients)
- Familiarizing yourself with the kit/ equipment available at your work location
- Practicing (and ideally simulating) the workflow of your preferred difficult airway management algorithm
- Practicing transtracheal injection for tracheal topical local anesthesia. Some anesthesia providers include transtracheal injection of a local anesthetic into their awake fiberopitc intubation preparation routine. Transtracheal injection can also be indicated in patients under general anesthesia if intubation is to be achieved without muscle relaxation.
Some anesthesia and emergency medicine conferences offer (human or animal) cadaveric courses covering FONA. Manikins and laryngeal models are also availabe for FONA training. You can make low-fidelity models yourself when the emphasis is not anatomically correct modelling but allowing to practice the steps of your preferred technique.
REFERENCES
Edelman, D. A.; Perkins, E. J.; Brewster, D. J. (2019): Difficult airway management algorithms: a directed review. In Anaesthesia 74 (9), pp. 1175–1185. DOI: 10.1111/anae.14779.Price, T. M.; McCoy, E. P. (2019): Emergency front of neck access in airway management. In BJA Education 19 (8), pp. 246–253. DOI: 10.1016/j.bjae.2019.04.002.