Definition
Although there is no rock-solid definition as to what consitutes a 'difficult' airway, it is generally understood to mean difficulty with ...
- Laryngoscopy and intubation, and more importantly ...
-
ventilation, i.e. oxygenation, which means problems with ...
- bag-mask ventilation
- oxygenation with a supraglottic airway as a rescue technique, and might require
- oxygenation with a FONA (front-of-neck airway) as a last resort
... after induction of general anesthesia.
However, it is easy to ignore the fact that airway 'diificulties' commonly present on emergence from general anesthesia and with extubation (Cavallone et. al., 2013). In fact, the NAP4 audit found that a third of adverse events in airway management occured during extubation or after emergence!
CAUTION: Between difficult oxygenation and difficult intubation, (anticipated or actual) problems with oxygenation are more concerning!
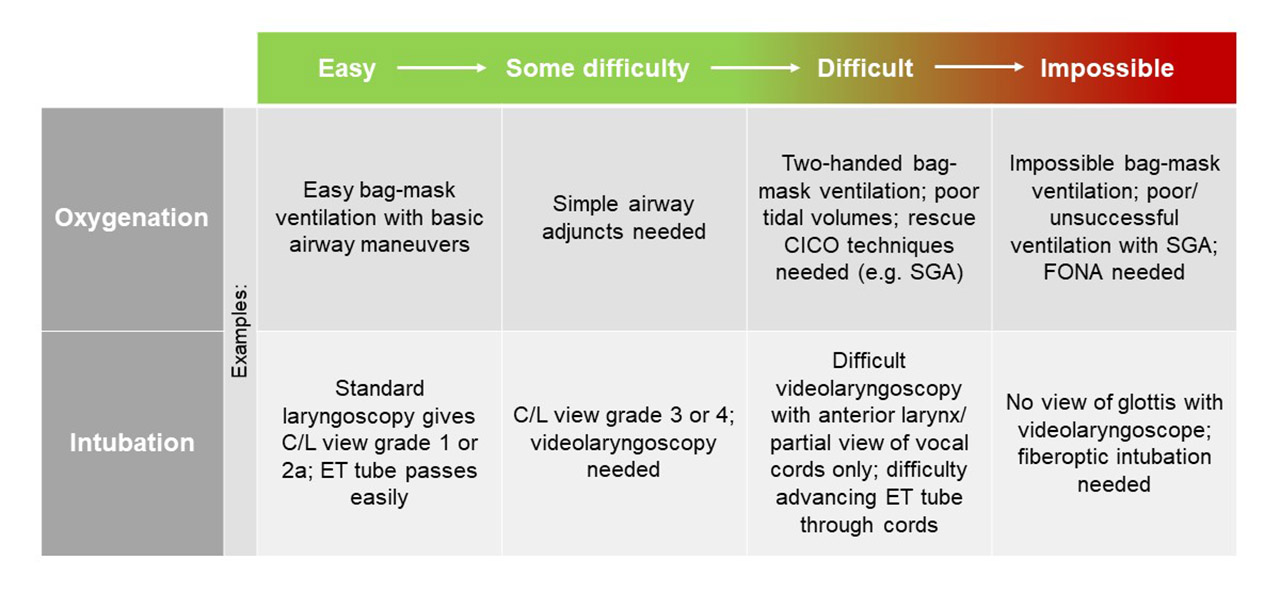
There clearly is a spectrum of 'difficulty' with regards to both oxygenation and intubation, ranging from maybe some difficulty with bag-mask ventilation requiring simple airway adjuncts to a CICO scenario requiring emergency FONA (see table below).
The anticipated vs. unanticipated difficult airway
Anticipated difficult airway
If a difficult airway is 'anticipated' (based on your thorough preoperative airway assessment!), it allows for the formulation of a safe airway management strategy before you put the patient to sleep. You will have enough time to devise a 'Plan A' and a 'Plan B' for your airway management, gather needed equipment and help ahead of time. While airway management can still be challenging, it should happen in a fairly controlled fashion.
It is helpful to note the difference between making or having an airway plan and an airway strategy:
- Airway plan: Making an airway plan means coming up with a 'Plan A' for airway management. In contrast to an airway strategy, an airway plan considers just one primary approach with the expectation that it will succeed. This is not good enough since it is a 'failure to plan for failure'. Example for an airway plan: "I will induce general anesthesia and insert a size 4.0 igel SGA".
- Airway strategy: Having an airway strategy on the other hand means anticipating problems with your primary airway plan, considering and planning for alternatives and rescue techniques should your airway 'Plan A' fail. It essentially means having a 'Plan B', and sometimes a 'Plan C' in place before you start airway management. Example for an airway strategy: "I will induce general anesthesia and insert a size 4.0 igel SGA. If the seal is poor I plan to change this to a size 5.0 igel SGA, and in case this does not work, proceed to muscle relaxation and intubation."
CAUTION: Always have an airway strategy, don't just make an airway plan! The more difficulties you expect in management of the airway, the more you need to think about your airway strategy.
Unanticipated difficult airway
In contrast to the anticipated difficult airway this will be a more or less challenging surprise to you after induction of general anesthesia. Having to deal with an unanticipated difficult airway can be very stressful, especially in patients in whom oxygenation is difficult and who develop rapidly worsening hypoxia. An easy-to-remember management algorithm for the unanticipated difficult airway such as the VORTEX approach (see below) is extremely helpful in those situations, will help you to focus and take the correct actions when your capacity for calm rational thought and planning might be impaired.
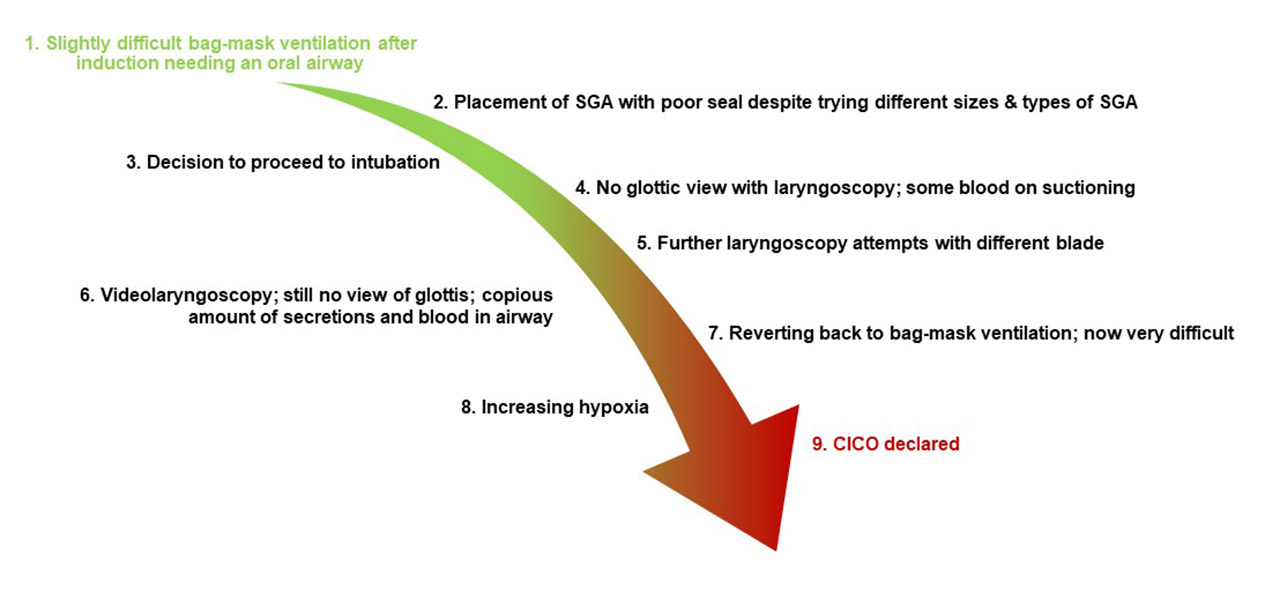
Often an unanticipated difficult airway does not start out as such. In many instances an airway which is initially, after GA induction, manageable if slightly difficult, deteriorates with repeated management attempts (see clinical example below). In fact, this is probably a more likely scenario than that of an unanticipated airway with very difficult or impossible oxygenation and intubation encountered immediately after induction.
In the scenario described below, oxygenation is initially manageable, only intubation is difficult. To begin with, this is therefore a stable, controlled situation since oxygenation is possible. With bag-mask ventilation as a fall-back technique being possible, there is no rush to intubate. Then, however, with repeated intubation and airway instrumentation attempts, it becomes increasingly difficult to even oxygenate the patient, which is much more dangerous that difficulty to intubate. This has now turned into a much more unstable, uncontrolled situation.
Management algorithms for the unanticipated difficult airway
It is absolutely essential to be familiar with (at least one) management algorithm for the unanticipated difficult airway and follow its strategy should the situation occur. Several specialist societies from a number of countries have published their own guidelines and algorithms (Edelman et al., 2019).
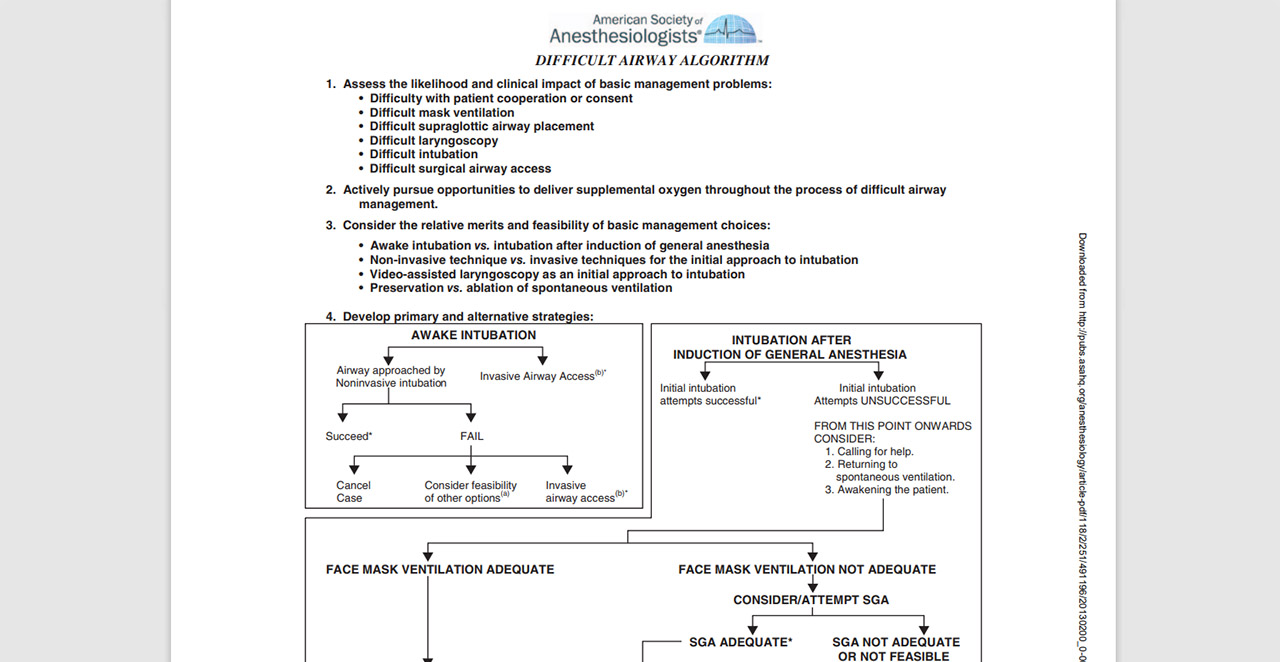
As examples, these are guidelines from the UK, Australia and the US:
United Kingdom
The Difficult Airway Society (DAS) presents its guidelines on their website, which is a highly recommended resource.
Australia
From an Australian group comes the VORTEX approach to managing the (unanticiated) difficult airway. Please visit their excellent website!
PERSONAL OPINION: I think the VORTEX approach, which is widely taught in Australia, is particularly useful since it is easy to remember in an emergency because of its simple logical visual approach. It is what we teach our trainees. The DAS guidelines and the website on which thet are published are also excellent. The ASA guidelines include a nice review and grading of available evidence and expert opinion. As a practical clinical decision-making tool I feel they are not as good as the VORTEX and DAS guidance. The ASA algorithm looks somewhat confusing with a messy layout and can be difficult to recall in a high-stress situation such as a CICO scenario (an update is currently in the works).
Common features of management algorithms for the unanticipated difficult airway
While there are notable differences between algorithms from various sources, some elements seem common to most management guidelines of the unanticipated difficult airway:
- The primary goal is to achieve and/ or maintain oxygenation rather than intubation.
- There are generally three options for oxygenation in the unanticipated difficult airway: 1. Bag-mask ventilation, 2. supraglottic airway, and 3. intubation. FONA is the rescue technique if these three don't work. The VORTEX approach calls these options the three 'lifelines'.
- With regards to the three oxygenation options or 'lifelines', pretty much all algorithms emphasize to not keep trying the exact same thing over and over again if unsuccessful and to limit the total number of attempts at any one 'lifeline' before you move on to a different one (and finally consider FONA). Several guidelines recommend no more than three attempts at each lifeline, with each one "incorporating additional optimisations that have not previously been implemented" for a "best effort" to quote the VORTEX approach.
- FONA is the only rescue technique should all other attempts at oxygenation fail, i.e. a CICO scenario occur.
- Muscle relaxation is increasingly suggested when difficulty with oxygenation is encountered. DAS guidance and the VORTEX make an explicit recommendation to paralyze. Not all guidelines support this though!
- Consider waking the patient up (if it is an option).
- Mentally prepare for the possibility of CICO and need for FONA early. Clearly only very few unanticipated difficult airways end up in a CICO scenario. However, if you find yourself going through and exhausting the three options for oxygenation without success, mentally prepare for the fact that FONA might be required within the next minute to prevent hypoxic brain injury or patient death!
NAP4 lessons
If your clinical practice includes airway management and there is a possibility that you might encounter a difficult airway in your work, you need to be familiar with the most important findings of the 4th National Audit Project (NAP4) from the UK on 'Major Complications of Airway Management'. At the very least read the executive summary!
REFERENCES
Edelman, D. A.; Perkins, E. J.; Brewster, D. J. (2019): Difficult airway management algorithms: a directed review. In Anaesthesia 74 (9), pp. 1175–1185. DOI: 10.1111/anae.14779.

Add new comment