What is meant by 'intubation through an SGA' is exchanging one type of airway, i.e. a supraglottic airway (SGA), for another (endotracheal tube) without having no airway in-situ at any time during the exchange.
INDICATIONS
This technique can be useful in a number of situations:
1. After unsuccessful intubation attempts with direct laryngoscopy (and bougie)
If intubation with direct laryngoscopy (and bougie) has failed, for example due to a poor grade 3 C/L view of the larynx, an SGA can be placed temporarily for oxygenation/ anesthetic delivery which can then be used as a conduit for an endotracheal tube or an Aintree catheter (which will then be exchanged for an ET tube).
This assumes of course that bag-mask ventilation is possible. If not, you have a CICO scenario and need to follow an appropriate management algorithm!
Arguably, most practitioners would attempt videolaryngoscopy as a next step if direct laryngoscopy and bougie have failed, rather than use this approach straight away.
2. After unsuccessful intubation attempts with videolaryngoscopy
Videolaryngoscopy is often successful when direct laryngoscopy has failed, so this indication is rarer than the one above. But, if direct laryngoscopy and videolaryngoscopy have failed, SGA insertion followed by intubation is a logical next choice. Again, this assumes of course that bag-mask ventilation and therefore oxygenation is possible.
3. Intraoperative need for conversion from supraglottic airway to endotracheal tube
This could be a scenario where a change of surgical plan intra-operatively makes muscle relaxation necessary and the practitioner does not feel confident to ventilate a paralyzed patient with an SGA in-situ. This is probably only indicated if direct laryngoscopy and videolaryngoscopy have been unsuccessful (as described above). An easier and therefore first-choice approach would be to remove the SGA and then intubate with direct laryngoscopy or videolaryngoscopy.
(4. 'Can't-intubate-can't-oxygenate' (CICO) scenario with failed bag-mask ventilation but successful SGA rescue)
This would be a situation where a) bag-mask ventilation and intubation were unsuccessful, b) an SGA however allows oxygenation of the patient, c) there is a clinical need for securing the airway with an endotracheal tube rather than continue the case with the SGA, and d) the patient cannot immediately be woken up from general anesthesia.
A clinical example might be an emergent c-section for acute fetal distress under general anesthesia, where standard intubation has been impossible and oxygenation is (just about) possible with an SGA. In this unlikely scenario delivery cannot be postponed (i.e. no patient wake up) and there is a high aspiration risk (i.e. endotracheal tube is required).
PERSONAL OPINION and CAUTION: I have put this indication (no. 4) in brackets for a reason: The risk of losing an already difficult airway completely (which will require immediate FONA) by manipulating it with a fiberoptic scope and endotracheal tube is almost always higher than a potential aspiration risk when continuing a case with an SGA. I would generally advise against considering this an appropriate indication for intubating through an SGA!
The table below summarizes where intubation through an SGA could fit into a management approach of failed intubation with direct laryngoscopy and/ or videolaryngoscopy (but successful oxygenation with bag-mask ventilation). Note that this is NOT talking about a CICO scenario because bag-mask ventilation IS possible! Also, this is not an exhaustive description of available options.
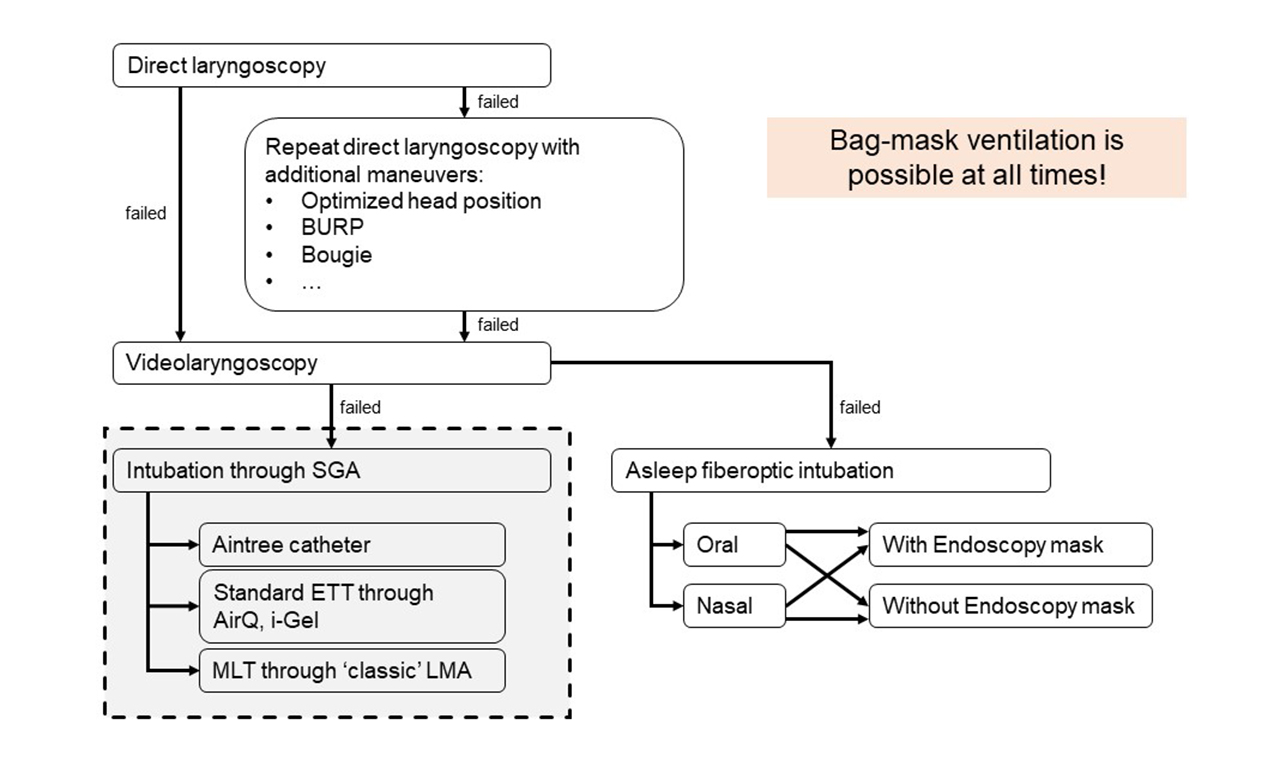
Intubation through an SGA versus asleep fiberoptic intubation
An alternative approach to intubating through an SGA is asleep fiberoptic intubation. However, intubation through an SGA has a couple of advantages and no real disadvantages compared to the simple asleep fiberoptic intubation approach:
- An SGA acts as a soft tissue bypass in the posterior pharynx and 'guides' the scope towards the larynx. It might be easier to obtain a view of larynx from the distal opening of an SGA than by advancing a scope through the oral cavity, oropharynx and hypopharynx without a conduit or a even a Berman or Ovassapian airway.
- Oxygenation can continue longer through the in-situ SGA and the period of apnea is shorter compared to the asleep fiberoptic intubation approach (unless maybe an Endoscopy mask is used).
CAUTION: Always remember that repeated failed laryngoscopy/ intubation attempts and airway instrumentation of any kind can quickly convert a 'maskable' airway into a CICO scenario!
EQUIPMENT
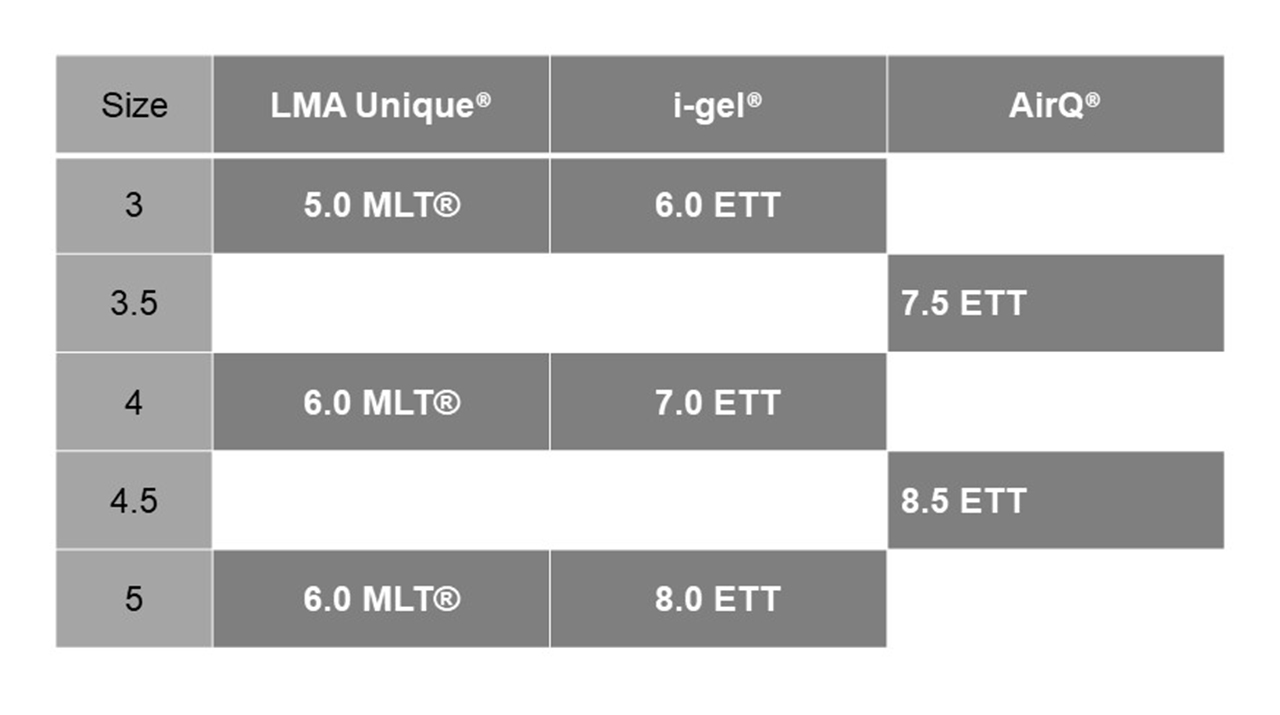
Obviously, not all endotracheal tubes can be passed through all sizes and types of SGAs. Please refer to the table below to see what fits what.
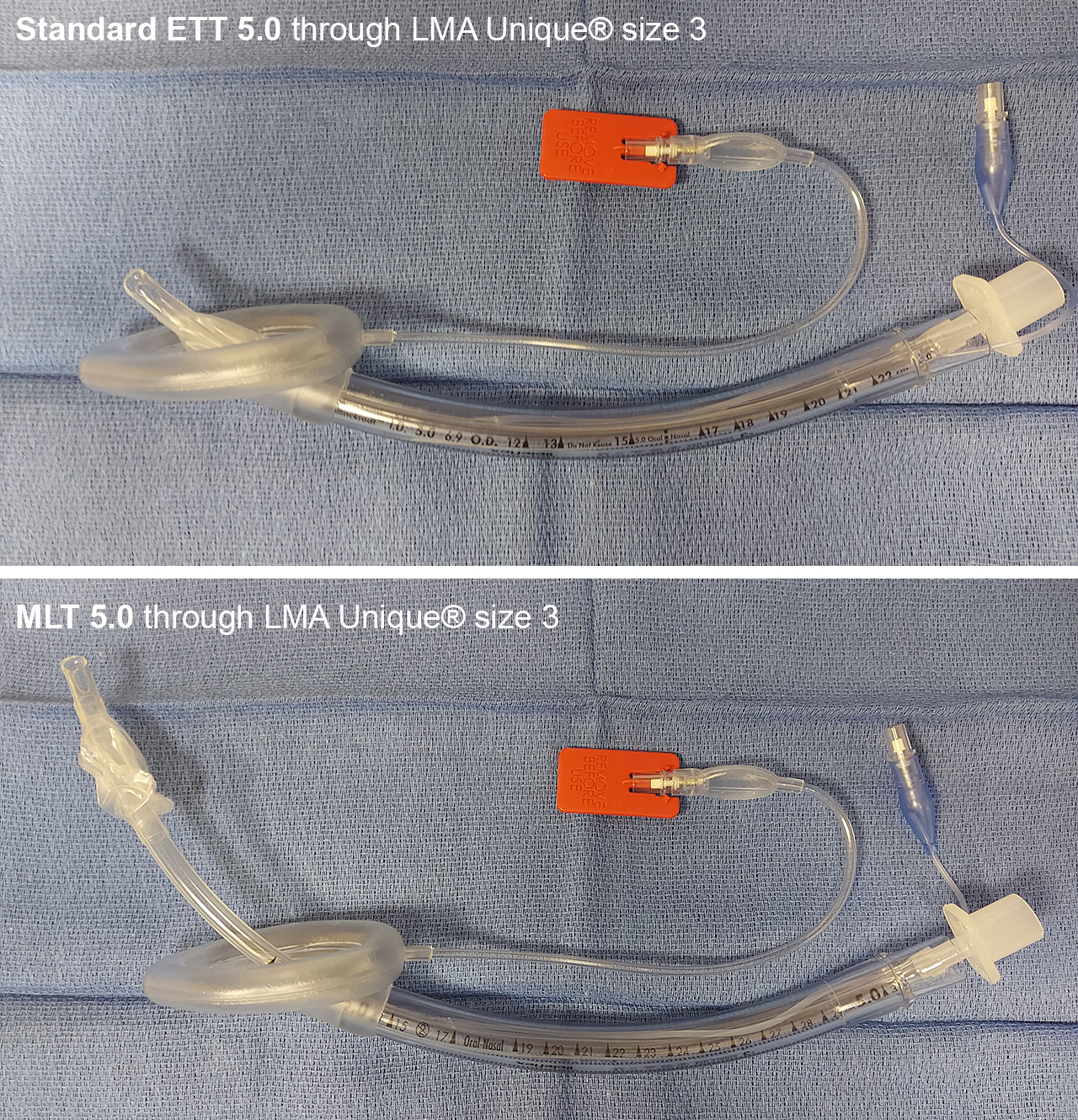
While the LMA Unique® can accomodate standard ET tubes, for the maximum suitable sized ETTs tend to be too short to allow for reliable pass of the cuff below the vocal cords. This is why the longer MLTs® are needed if used in conjuction with the classic design LMA Unique®:
TECHNIQUES
Several techniques are available for intubation through a supraglottic airway (SGA). We describe the first three on the linked pages:
- Fiberoptically-guided exchange of the SGA for an ET tube over an Aintree catheter (actually not an intubation through an SGA!)
- Advancing a microlaryngoscopy tube (MLT®) through an SGA
- Intubation through an AirQ SGA
- LMA Fastrach®
- ...
Techniques 1- 3 should always be used with fiberoptic guidance.
Add new comment